The treatment of Interstitial Cystitis/Bladder Pain Syndrome (IC/BPS)
Most guidelines – including the one of American Urological Association (AUA) – shares the view that the doctor should start with the least invasive method and progress step by step towards the more invasive technics.[1]
Lifestyle Changes and Diet
The least invasive therapeutic possibilities describe lifestyle changes. Diet has a major impact on the symptoms. IC/BPS food and drink lists are widely available on the internet,[2],[3],[4] and scientific papers have been published about this topic, too.[5],[6] Most of the references agree that certain nourishments irritate the damaged bladder wall. Lists usually mention the following things:
- Caffeinated beverages
- Alcoholic drinks
- Hot and spicy foods
- Sour and acidic foods, including carbonated drinks
- Some fruit of high acid content
- Tea or certain dietary supplements containing fragrance oil and/or volatile oil compounds
- Herbal products
Indeed, following an IC/BPS-friendly diet can help mitigate the symptoms. However, lifestyle and diet changes alone do not always work, especially in severe cases. It usually takes a considerable amount of time until the effects manifest, and during this sort of therapy, the symptoms may become worse.
Oral Medication
If there is no improvement experienced, the next major line of treatment is oral therapy. The most common medicines usually contain one or more of the following active ingredients:
- Antihistaminic anti-inflammatories
- Non-steroidal anti-inflammatories
- Corticosteroid anti-inflammatories
- Tricyclic antidepressants
- Gabapentin nerve pain relieve
It must be pointed out that the list of approved – and available – products greatly varies by country.
There have been plenty of studies examining the efficacy of these substances, it is summarized on many pages, too.[7] These agents have anti-inflammatory, pain mediator blocking and antidepressant effect; therefore, oral medication is an effective way of mitigating the urinary and/or the pain symptoms, thus improving the patient's quality of life.
Urine alkalization is an important part of the oral treatment, too, since the acidic urine can irritate the bladder and make the symptoms worse. Avoiding food groups that make the urine more acidic is not effective enough in many cases. Therefore, alkalizing pills (medicines or food supplements) play a major role in oral medication, as well.
These agents, however, have little to no effect on the integrity of the GAG-layer. It is worth mentioning there are certain products which do contain one or more active pharmaceutical ingredients (detailed later) used for GAG-layer replenishment. Many of them are widely known and available on the internet. In this group, the most important medicine is Pentosan Polysulfate Sodium (PPS, Elmiron, SP-54), which is approved by the Food and Drug Administration (FDA, the USA), and considered to be the only oral drug that actively helps GAG-layer replenishment.
Regardless of using GAG-layer replenishment agents, oral therapy has some considerable drawbacks. To reach the bladder the drugs must be absorbed in the digestive system, enter the circulation and reach other tissues too. This fact lowers the efficacy of the drugs and increases the chance of side effects. PPS, for example, has to be taken for 3 months or more to experience its effect on the GAG-layer. Orally administered PPS taken over longer period may have serious side-effects;[8] a recent discovery on this topic is particularly concerning.[9]
Local Treatment (Intravesical Instillation)
The next possibility is the local treatment, which means instilling certain substances directly into the bladder.
In the last 20 years there have been plenty of active agents tried out. Some of these, for example BCG (Bacillus Calmette-Guarin) have turned out to be ineffective.[10] Others, like interfering with the nerve growth factors, have had safety issues.[11] With certain substances, only partial improvement has been achieved: with vanilloids, for example, pain have had been reduced, but no improvement has been observed regarding the urinary symptoms.[12] There are some agents which have been under examination right now, but either the results have been controversial and/or inconclusive so far, or there have not been enough clinical tests yet. Blocking the P2X3 receptors (which affect the bladder activity) might be promising, but further experiments would be needed.[13] Botulinum toxin A (BTX-A, Botox) has been examined several times, but the results seem controversial.[14],[15] Using liposomes for delivering different agents might be an efficient method,[16] but, again, further experiments would be needed.
Regarding the active ingredients, there are six major compounds which that are associated with GAG-layer replenishment. These are the following:
- Pentosan polysulphate sodium (PPS, Elmiron, SP-54)
- Dimethyl sulfoxide (DMSO, Rimso-50)
- Lidocaine (alkalized lidocaine, AL)
- Heparin
- Hyaluronic acid (HA)
- Chondroitin sulphate (CS)
The clinical data on these substances are, on the other hand, controversial.
The structure of PPS is similar to those compounds which are naturally present in the GAG-layer. Its mechanism of action is still not known, but it might be an effective intravesical medicine.[17]
DMSO is the only drug that is approved by the FDA for bladder instillation. According to some papers, it is more effective than certain other agents,[18] whereas other references point out the issues related to DMSO.[19]
Alkalized lidocaine (AL) is often used in different bladder cocktails. According to certain sources, it is an effective medicine for GAG-layer replenishment[20] on its own. Most therapists think it can raise the efficacy of other compounds,[21] even if there are studies denying it.
Heparin, hyaluronic acid and chondroitin sulphate are natural components of the GAG-layer. Heparin, either alone or with other compounds is often used in the local treatment.[22] There are data that says it is less effective than e.g. DMSO (see above). Hyaluronic acid may be the most widespread component; its efficacy has been examined several times, with different results.[23],[24],[25] The available data are similarly controversial for chondroitin sulphate, too.[26],[27],[28] According to some studies, HA+CS might be just as effective as DMSO.[29]
In practice, different therapists use different bladder cocktails,[30] hoping that the patient will respond to the treatment.
The large number of controversial data might be based on several facts. Firstly, the etiology of IC/BPS is still not known. If the disease can appear for different reasons, patients with different etiology might respond differently to the treatments. Secondly, in many countries only one or very few of these medicines are approved, which alone hinders the possibility of building an objective and comparative picture. Thirdly, in most countries there are only a few agents or cocktails used for instillation, usually in a magistral form, which makes it very hard to run clinical trials with ample sample sizes.
It is worth examining why local treatment is less popular to oral medication in spite of it is more effective – providing the right medicine is used. Invasiveness is an important factor. Many doctors tend to avoid using a catheter unless it is inevitable. Patients often refuse instillation therapy, being afraid of the pain, and the risk of further issues – microlesions and infections – a catheter can cause. To overcome these problems, Urosystem has developed UroDapter® and UroStill®. The former one is a small device which that replaces the catheter. The latter one is a device that enables self-instillation for female patients. With UroStill® the bladder treatment can be performed at home, without any direct assistance from the therapist.
Combined Therapy
It is inarguable that the first lines of the treatment – the less invasive methods, such as diet and oral medication – are necessary. Unfortunately, not only does the diagnosis take a long time, but also the effect of the less invasive therapies appears later. This leads to a common situation in which the patients waste 1–3 years or more living with hardly tolerable pain, severe urinary syndromes and a gradually worsening quality of life. The more time has been spent in this way, the more likely it is that the patient will not respond to the less invasive lines of treatment at all.
Our recommendations are summarized in the following flowchart. In cases of severe symptoms, it is recommended to start with combined therapy of oral and intravesical treatments so that the patient's condition can improve as soon as it can.
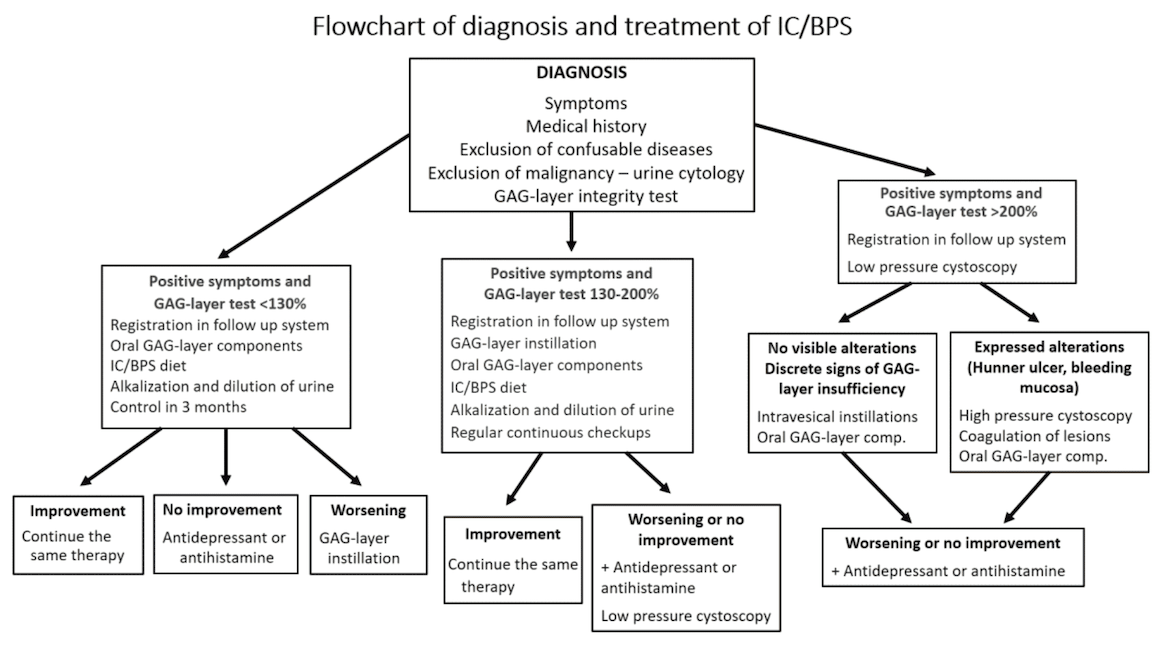
As it is shown, the applied line of treatment depends on the findings of the GAG-layer integrity test. Lifestyle changes, diet and oral medication is efficient and sufficient only in mild cases of IC/BPS. Patient follow-up is necessary in these cases, too, because despite the applied treatments a worsening condition cannot be ruled out. (The patient follow-up system has not been implemented to this website yet.)
At more severe conditions the GAG-layer replenishment via bladder instillations shall be started immediately, but all the less invasive methods are usually performed simultaneously.
More invasive therapies – including nerve stimulation, fulguration of the damaged regions of the GAG-layer or cystectomy – are performed only if all the other treatments have been ineffective. Alternative methods – including acupuncture, high-pressure oxygen therapy – are mostly recommended as supplementary treatments, taking into consideration their wrong cost-benefit ratio.